Posted on January 27, 2025 by Storm Goodman
There are many labs across the Klesse College of Engineering and Integrated Design, all filled with amazing projects and the extraordinary people who bring them to life. The Klesse College Field Trips series is dedicated to highlighting the work conducted in these labs, and so we are excited to share yet another fascinating lab. Join us as we explore Gabriela Romero Uribe’s Macromolecular Laboratory.
Brain-related diseases often stem from complications in brain cells’ ability to communicate with each other. With the complexity of the human brain, even tiny efforts to remedy these miscommunications can have numerous side effects and pose huge risks to the patient. However, Gabriela Romero Uribe and her team of researchers may have found a cutting-edge, non-invasive way to help treat patients suffering from these ailments. Utilizing nanotechnology capable of generating electricity to stimulate the brain cells, the team theorizes that they can correct the misfiring brain cells with minimal risks to the patient.
What type of research takes place in your lab?
GRU: My research team is working on developing bioelectronic medicines, which are a new type of treatment. We're focusing on using tiny, advanced technologies (nanotech) to safely stimulate the brain and nervous system without needing to make big cuts or use wires.
Malfunctions in the brain happen when communication between brain cells, or neurons, goes wrong. Imagine the brain as the Christmas lights in your tree, where each light represents a cell, and all cells relate to each other in series creating your “brain lights”. When everything is working well, electricity travels smoothly through the series brightening each light, which allows the brain to control things like movement, thoughts, and emotions. But sometimes, one "light series" gets damaged, impeding the electricity from continuing flowing. This can cause the brain to send wrong signals or miss important ones, leading to problems like memory loss, difficulty moving, mood swings, or even things like seizures. In other words, the brain's "lights" aren't working the way they're supposed to, and this can result in conditions like Alzheimer's, Parkinson's, or other brain-related diseases.
The tools we develop in my research team help scientists better understand how brain cells (neurons) work, both when things are normal and when there are problems. Our work also leads to new ways to treat diseases of the brain and nervous system.
What is the thing in your lab that you are most proud of?
GRU: I am incredibly proud of the team of young researchers I’ve built at UTSA. This group of postdocs, graduate students, undergraduates, and sometimes even high school students and teachers has created a strong, supportive community where everyone helps each other learn and grow in their careers. The postdocs are the most experienced members of the team. They not only have the freedom to explore their own research ideas but also guide graduate students, offering advice on how to approach research, interpret results, and build their professional skills. The graduate students, in turn, serve as role models for the undergraduates and high school students, teaching them the basics of research and how to succeed in the field.
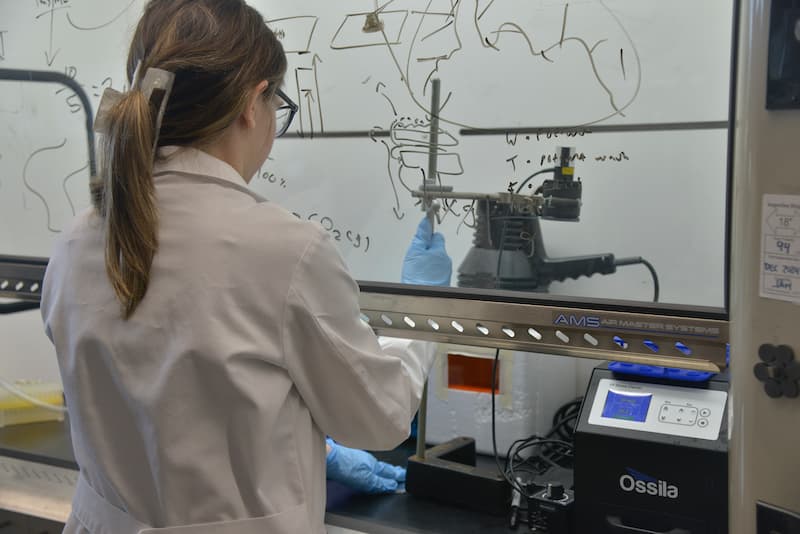
Together, this amazing team has made great strides in developing less invasive methods to treat problems in the brain and nervous system. We’ve created innovative technologies for wireless brain stimulation and come up with safer ways to get treatments into the brain, by passing the blood-brain barrier. Our team works with biomedical materials that can convert outside magnetic signals into responses that brain cells can understand like heat, electricity, or pressure. To build these technologies, we also design custom equipment to stimulate the brain using magnetic fields, along with a fast-recording camera that lets us watch and study how brain cells react in real time.
Which students (major and level: UG, GRAD, PhD) use your lab?
GRU: Undergraduate, Masters and PhD students from Biomedical Engineering and Chemical Engineering study in my lab.
What type of funding did you receive to stock your lab with the existing equipment?
GRU: UTSA startup funds, NIH NIGMS, NIH NINDS, NIH NIBIB, NSF MRI, NSF CAREER award, San Antonio Area Foundation Biomedical Grant

How does your lab help UTSA stand out from other engineering colleges?
GRU: My research team is truly one-of-a-kind at UTSA. We’re the only lab here focused on developing neuroengineering tools for brain stimulation, making our work distinct and highly specialized. We’re pioneering many of the technologies we create, and there are very few research groups—either in the U.S. or globally—that are exploring this cutting-edge field of bioelectronic medicine. This uniqueness not only sets us apart but also enhances UTSA’s visibility on the national and international research stages.
Anything else of interest?
GRU: Bioelectronic medicines could completely change the way we treat diseases by offering a more precise and less invasive approach. Instead of relying on pills or surgeries, these treatments use small electrical signals to fix problems in the body, directly targeting the nerves or tissues that need attention. For example, conditions like chronic pain, epilepsy, or even depression might be treated by adjusting the electrical activity in the brain or nervous system, perhaps using the technologies that my team develops. This could mean fewer side effects and longer-lasting results compared to traditional treatments. As this technology advances, it could allow doctors to customize treatments for each person, making healthcare more personal and effective. In the future, bioelectronic medicines could help repair and restore health in ways we never thought possible.

